WAAW: RSTMH small grants fund research to tackle AMR
World Antibiotic Awareness Week
World Antimicrobial Awareness Week (WAAW) is a week devoted to increasing awareness of global antimicrobial resistance (AMR) and to encourage best practice among the general public, health workers and policy makers to avoid the further emergence and spread of drug-resistant infections. Antimicrobials is broad term covering antibiotics, antivirals, antifungals and antiparasitic medication.
AMR is a global health and development threat. The World Health Organization (WHO) has declared that AMR is one of the top 10 global public health threats facing humanity with significant costs to economies. Prolonged illness results in longer hospital stays and the need for more expensive medicines. Without effective antimicrobials, the success of modern medicine in treating infections, including during major surgery and cancer chemotherapy, would be at increased risk.
There are a number of reasons why AMR is increasing. These include inappropriate use of antimicrobials in humans, livestock and agriculture, and these are the main causes of the development of drug-resistant infections.
Poor stewardship is also a contributory factor. Furthermore, a lack of clean water and sanitation in healthcare facilities, farms and community settings promotes the development and spread of drug-resistant infections in addition to inadequate infection prevention and control.
Putting antimicrobial awareness front and centre
In 2020, we awarded 124 small grants to early career researchers, several of which focus on antimicrobial resistance.
We asked three small grant awardees working in this space to talk about their research.
Aparna Ananthakrishnan

Aparna Ananthakrishnan, "Reviewing Evidence on Economic Evaluations of Interventions and Policies to Address Antimicrobial Resistance in Low- and Middle-Income Countries".
Aparna is an Overseas Development Institute Fellow at the Health Intervention and Technology Assessment Program, Ministry of Public Health, Thailand. She supports capacity building efforts for improved evidence-informed decision making in low-and middle-income countries (LMICs).
She has previously assisted with research on neglected tropical disease outbreaks and treatments, informing programme implementation for deworming in countries across South Asia and Sub-Saharan Africa at Evidence Action in Washington DC, where she was a Global Health Corps Fellow.
Why is your research needed?
"Over the past decade, several countries, including LMICs, have started implementing interventions to tackle AMR. However, economic evidence regarding the cost-effectiveness of these interventions remains weak. This evidence gap particularly impacts resource-constrained settings such as LMICs which face competing budgetary priorities.
"Most importantly, this review may help re-emphasise that more research is required to bolster economic evidence on AMR interventions, especially as we battle a virulent pandemic and reflect on broader issues of global health security for our future."
What is the aim of your project?
"There are three aims: a systematic literature review to look at review the global evidence on the cost-effectiveness of different AMR interventions, as well as a policy survey to identify which interventions are implemented in LMICs and how they might compare against existing cost-effectiveness evidence, therefore informing future policy and research priorities for AMR control in LMICs."
What will be the impact of your research?
"The review will be one of the first of its kind to systematically review the literature on the cost-effectiveness of AMR interventions, an important evidence gap in the economics of AMR.
"This review may also help guide other evidence-generating activities (such as the need for better evidence regarding the effectiveness of interventions or costing information, both in general and in specific contexts such as LMICs). The findings of this systematic review alongside the findings of the survey will enable policy and decision-makers, particularly in resource-constrained settings, to better use available resources when selecting interventions to address AMR burdens."
Love Omoniyei

Love Omoniyei, "Assessment of Antibiotic Prescribing Patterns Using WHO Access, Watch, and Reserve Classification in Outpatient Pharmacies Across Hospitals in Abuja, Nigeria"
Love is a pharmacist and project supervisor at Ducit Blue Solutions, a healthcare consultancy company in Abuja. He is a member of Nigeria’s AMR and Risk Communication Technical Working Group at the Nigeria Centre for Disease Control and supports the team to carry out implementation activities in the country.
He has a special interest in health systems strengthening towards provision of equitable, accessible and affordable healthcare, especially in LMICs.
Why is your research needed?
"Little information is available on antimicrobial use in low-income countries, especially Nigeria. This research is particularly useful in this part of the world as the evidence shows a dearth of studies.
"The WHO recently demonstrated the use of the access, watch, and reserve (AWaRe) index in the analysis and interpretation of global antibiotic consumption data. Hence this research is timely, as it supports the WHO call for use of the AWaRe index by WHO member states to estimate the relative use of narrow-spectrum and broad-spectrum antibiotics, to aid evaluation of progress in optimising antibiotic use and to help in defining goals for future quality improvement.
"This information on prescribing will further serve as a benchmark to target antibiotic stewardship intervention and assessment of trends over time."
What is the aim of your project?
"The project aims to assess antibiotic prescribing patterns using WHO AWaRe antibiotic categories as a metric in outpatient pharmacies across two secondary health facilities in Abuja."
What will be the impact of your research?
"It is expected that the study would provide baseline hospital level data on pertinent antibiotics use across hospitals in the Federal Capital Territory Abuja (FCTA). This research can inform future interventions for healthcare workers in the FCTA such as continuing professional development courses and antimicrobial stewardship training.
"It will provide high level understanding of antibiotic prescribing and will be used to inform policies, regulations and interventions to optimise the use of antibiotics. Finally, the results of this project will be available to hospital management boards and AMR National Secretariat."
Richard Nyeko
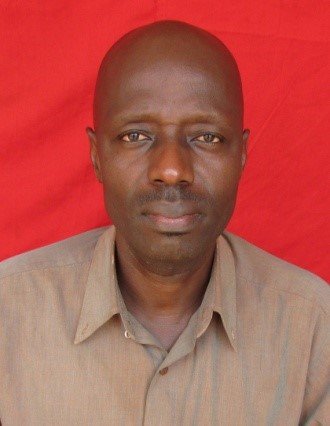
Richard Nyeko, "Pre-hospital antibiotics exposure among febrile children presenting to a tertiary health-facility in northern Uganda: prevalence, microbial correlates and resistance patterns"
Richard is a paediatrician and a public health specialist who obtained his qualifications from Makerere University, Uganda. His experience is in clinical practice in low-resource contexts and he has a strong interest in child health research.
Why is your research needed?
"The extent of inappropriate use of antibiotics for home treatment of fever in children and its significance in the era of emerging resistance to most available antibiotics has not been well elucidated in the current study setting. Literature reporting the burden of non-prescribed pre-hospital antibiotic exposure in children with fever is largely lacking.
"In this study, we will seek to bridge this important knowledge gap, in the hope of contributing to the better handling of antibiotics and management of illnesses and infections in children. It is expected that this will ultimately help to address the challenge of antibiotic resistance and protect available antibiotics from the pressure and emergence of resistant bacterial strains threatening to render them ineffective."
What is the aim of your project?
"The aims of this project are to determine the prevalence of pre-hospital exposure to antibiotics among febrile children presenting to a tertiary health facility in northern Uganda and to establish the microbial correlates and resistance patterns."
What will be the impact of your research?
"Understanding the magnitude, drivers and contribution of antibiotic use among febrile children on the current burden of antimicrobial resistance is expected to lead to a better public health approach in addressing the practice and consequently diminishing inappropriate exposure to antibiotics.
"The impact of this will ultimately be the protection of the available, as well as future, antibiotics from the pressure and emergence of resistant bacterial strains that threaten to render them ineffective."
We all have a role in tackling AMR
In partnership with the National Institute for Health Research, we are delighted to be supporting these three grants.
Everyone can play an important part in helping to limit the rise of AMR, such as regularly washing hands, recognising that antibiotics only work against bacteria (they are ineffective against viruses such as cold and flu viruses and the COVID-19 virus), and following your health professional’s instructions when they prescribe antibiotics for you.
